Pediatric fever of uncertain source
Revisión del 18:10 20 abr 2022 de Rossdonaldson1 (discusión | contribs.) (/* Initial Empiric Antibiotics for Well-Appearing InfantsEvaluation and Management of Well-Appearing Febrile Infants 8 to 60 Days Old Robert H. Pantell, Kenneth B. Roberts, William G. Adams, Benard P. Dreyer, Nathan Kuppermann, Sean T. O'Leary, Kymika...)
Background
- Medicine is an art as well as science, practice clinical judgment when using guidelines
- Preemies: Count age by estimated postconception date (not by actual delivery date) for 1st-90d
- Fever accounts for 30% of pediatric visits
- Children <3 mo are immunocompromised- poor opsonization, poor IgG response to encapsulated bacteria, macrophage and neutrophil dysfunction, bone marrow insufficiency
- Serious bacterial illness (SBI) includes UTI, meningitis, pneumonia, bacteremia
| Age | 0-14 days | 14-28 days | 28-60 days (pre vaccine) | 28-60 days (post vaccine) | 60-90 days | > 90 days |
| Meningitis/SBI Prevalence | 1/10 | 1/20 | 1/100 | 1/1000 | 1/1000-10,000 | > 1/10,000 |
Facts and Figures
- Take parental report of confirmed fever at home seriously in the 0-28 day range, even if never febrile in ED, as this population has been shown to have rates of serious bacterial infection (SBI) as high as 4.7% and invasive bacterial infection (IBI) as high as 1.8%[1]
From ACEP's Clinical Policy on Pediatric Fevers[2]
- 7% of patients < 2 years old with fever have pneumonia, however the etiology (viral/bacterial) or even the presence of pneumonia has low inter-observer reliability even among pediatric radiologists
- 4% Prevalence of UTI with common other sources of fever (OM, viral URI, et cetera)
- 1.5-2% background prevalence of asymptomatic bacteriuria in healthy afebrile controls
- 0.3% Rate of occult bactremia with healthy, well-appearing child who has a fever 2-24 months
- 0.3% of previously well children aged 3-36 months who have a fever without a source will develop significant sequelae, 0.03% will develop sepsis or meningitis
Concomitant RSV or Influenza Infection
- Relatively high coincidence of bronchiolitis w/ UTI, and of enterovirus and paraflu w/ UTI and bacteremia
- In RSV+ (by PCR) neonates aged 0-28 days, 6.1% had UTIs and 3.7% were bactremic; there was no difference in rates of SBI between RSV+ and RSV- neonates in a large prospective multicenter study entailing 1,248 children[3]
- RSV+ infants aged 29-60 days, the SBI rate was 5.5%, all of which were UTIs
- Influenza+, low risk of bacterial illness
Evolving Practices for Febrile Infants 0-60 days (2019 JAMA Peds)[4]
- Prospective multicenter observational study with 1821 patients split into derivation and validation groups.
- Inclusion fever >38C in ED or in past 24 hours measured.
- Exclusion premature < 36 weeks, previously known diagnosis/illness, or severe illness.
- Incidence of SBI in cohort 9.3% (8.3% UTI)
- Following elements had 97.7% sensitivity and 60% specificity for infants at low risk of SBI using
- ANC of 4090 or less
- Procalcitonin 1.71 or less
- Negative urinalysis
- No cases of bacterial meningitis missed. 3 missed SBI, all of which were > 28 days.
- May lead to decreased unnecessary LPs, will have variable adoption pending further validated studies/applications.
Differential Diagnosis
Pediatric fever
- Upper respiratory infection (URI)
- UTI
- Sepsis
- Meningitis
- Febrile seizure
- Juvenile rheumatoid arthritis
- Pneumonia
- Acute otitis media
- Whooping cough
- Unclear source
- Kawasaki disease
- Neonatal HSV
- Specific virus
Evaluation & Management
0-7 Days
For all infants (toxic and well-appearing)
| Child Appearance | Work Up | Treatment | Disposition & Follow-up | Comments |
| Temperature ≥38°
Toxic or Well |
|
|
Admit | SBI incidence
|
^Acyclovir if:
Note:
- CXR is optional if no resp sx and another source identified
- LP is necessary even if another source identified due to immature blood-brain barrier
- Do not give ceftriaxone to children <28d as may cause hyperbilirubinemia
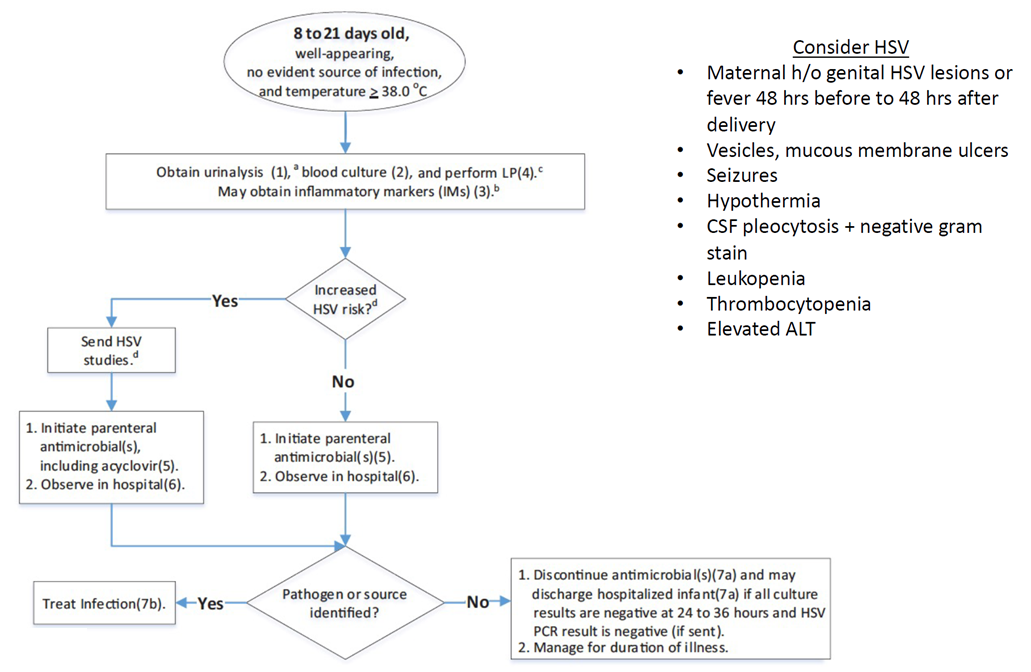
8-21 Days[5]
- For toxic infants, treat for sepsis and admit
- For well-appearing infants, see below algorithm
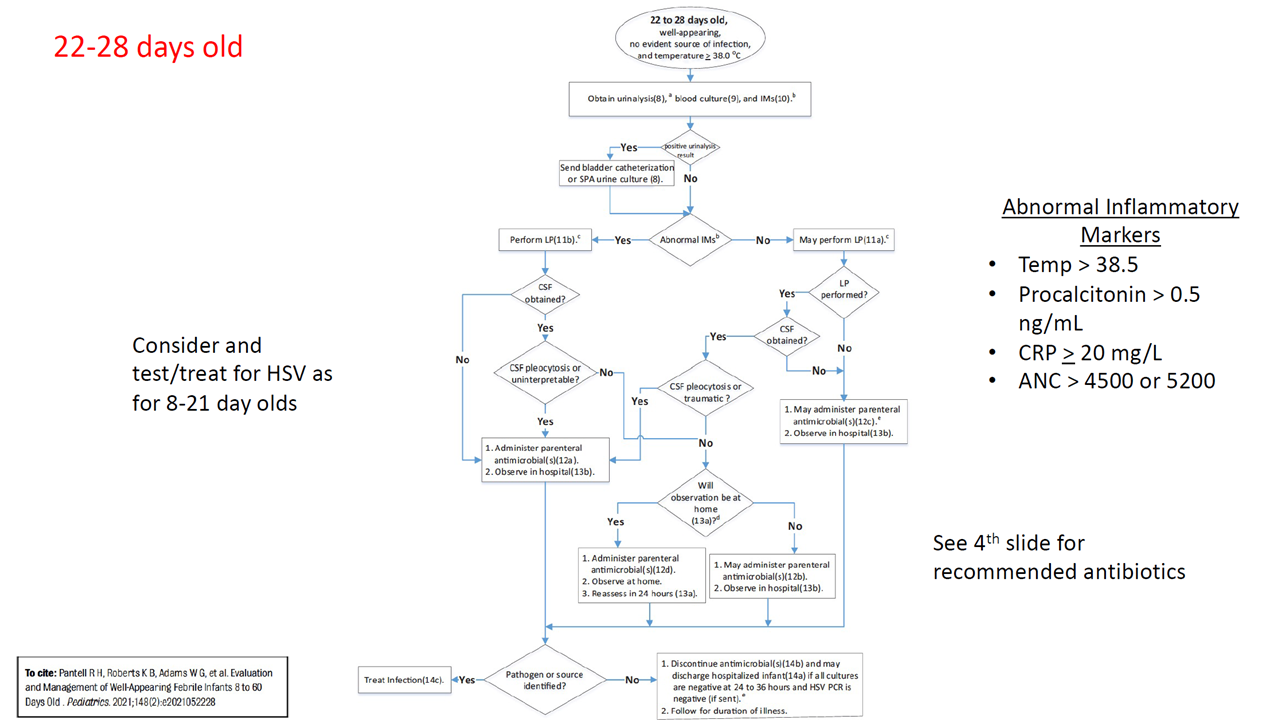
22-28 Days[6]
- For toxic infants, treat for sepsis and admit
- For well-appearing infants, see below algorithm
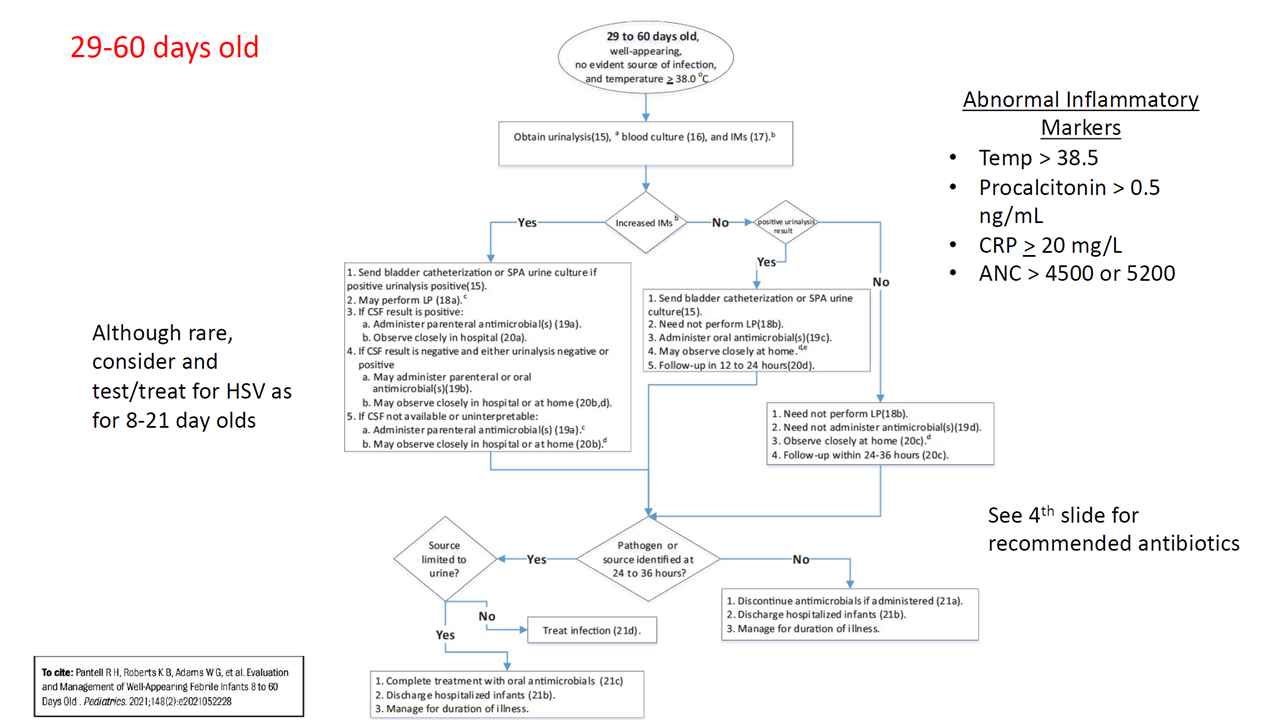
29-60 Days[7]
- For toxic infants, treat for sepsis and admit
- For well-appearing infants, see below algorithm
60 Days - 36 Months[8]
| Appearance | Work Up | Treatment | Disposition & Follow-Up |
| T≥38° + Toxic |
|
|
Admit |
| T≥39°C + Well + Non-complete Prevnar |
|
If WBC(+):
|
Outpatient (24 hour follow-up) |
| T≥39°C + Well + Prevnar |
|
Treat cystitis or pneumonia if postitive | Outpatient (48hour follow up) |
| T≥38-38.9°C + Well | Consider UA, CXR based on symptoms, etc | Treat cystitis or pneumonia if positive | Outpatient (48-72 hour follow-up)[9] |
- Consider CXR for:
- Respiratory symptoms
- Fever >48 hrs
- Tachypnea
- Hypoxia
- Non-UTI SBI incidence of <.4% in children >6 mo
Low Risk Lab Criteria
If low-risk criteria below not met, then perform the LP (if not done) and admit for inpatient antibiotics[10][11]
CBC
- WBC 5-15 /mm3
- Absolute Band count <1500 /mm3
Urinalysis
- Clear
- Neg Nitrate and Leukocyte esterase
- WBC <10/high powered field
CSF
0-28 days
- WBC: 0-22/mm3
- Protein: <100mg/dL
>29 days
- WBC 0-7/mm3
- Protein: 15-25mg/dL
Symptomatic Management
Initial Empiric Antibiotics for Well-Appearing Infants[12]
| Suspected Infection Source | 8-21 Days Old | 22-28 Days Old | 29-60 Days Old |
| UTI |
|
|
|
| No source identified |
|
|
|
| Bacterial meningitis |
|
|
|
Acetaminophen Pediatric Dosing Chart
| Weight (kg) | Weight (lbs) | Age | Dosage (mg) |
| 3-4 | 6-11 | 0-3 mo | 40 |
| 5-7 | 12-17 | 4-11 mo | 80 |
| 8-10 | 18-23 | 1-2 y | 120 |
| 11-15 | 24-35 | 2-3 y | 160 |
| 16-21 | 36-47 | 4-5 y | 240 |
| 22-26 | 48-59 | 6-8 y | 320 |
| 27-32 | 60-71 | 9-10 y | 400 |
| 33-43 | 72-95 | 11 y | 480 |
- Dosage can be given q6 hours
See Also
- Acute fever
- Fever of unknown origin (peds)
- Urinary tract infection (peds)
- Sepsis (peds)
- Meningitis (peds)
- Febrile seizure
External Links
References
- ↑ Serious bacterial infections in neonates presenting afebrile with history of fever Ramgopal S, Walker LW, Tavarez MM, et al. Pediatrics. 2019;144(2):e20183964.
- ↑ Clinical Policy for Children Younger Than Three Years Presenting to the Emergency Department With Fever. Annuals of Emergency Medicine 2003 42. 530-545
- ↑ Greenes, D.S.M., & Harper, M. B.M. (1999). Low risk of bacteremia in febrile children with recognizable viral syndromes. Pediatric Infectious Disease Journal, 18(3), 258-261.
- ↑ Kuppermann N, Dayan PS, Levine DA, et al. A Clinical Prediction Rule to Identify Febrile Infants 60 Days and Younger at Low Risk for Serious Bacterial Infections. JAMA Pediatrics. 2019;173(4):342-351. doi:10.1001/jamapediatrics.2018.5501
- ↑ Evaluation and Management of Well-Appearing Febrile Infants 8 to 60 Days Old Robert H. Pantell, Kenneth B. Roberts, William G. Adams, Benard P. Dreyer, Nathan Kuppermann, Sean T. O'Leary, Kymika Okechukwu and Charles R. Woods; Subcommittee On Febrile Infants Pediatrics July 2021, e2021052228; DOI: https://doi.org/10.1542/peds.2021-052228
- ↑ Evaluation and Management of Well-Appearing Febrile Infants 8 to 60 Days Old Robert H. Pantell, Kenneth B. Roberts, William G. Adams, Benard P. Dreyer, Nathan Kuppermann, Sean T. O'Leary, Kymika Okechukwu and Charles R. Woods; Subcommittee On Febrile Infants Pediatrics July 2021, e2021052228; DOI: https://doi.org/10.1542/peds.2021-052228
- ↑ Evaluation and Management of Well-Appearing Febrile Infants 8 to 60 Days Old Robert H. Pantell, Kenneth B. Roberts, William G. Adams, Benard P. Dreyer, Nathan Kuppermann, Sean T. O'Leary, Kymika Okechukwu and Charles R. Woods; Subcommittee On Febrile Infants Pediatrics July 2021, e2021052228; DOI: https://doi.org/10.1542/peds.2021-052228
- ↑ Jaskiewicz, J.A., McCarthy, C.A., Richardson, A.C., White, K.C., Fisher, D.J., Powell, K. R., et al. (1994). Febrile infants at low risk for serious bacterial infection-an appraisal of the Rochester criteria and implications for management. Pediatrics 94(3), 390-396.
- ↑ Baker, M.D., Bello, L.M., & Avner, J.R. (1993). Outpatient management without antibiotics of fever in selected infants. New England Jouranl of Medicine, 329(20), 1437-1441.
- ↑ Smitherman, H.F. & Macias, C.G. (2014). Evaluation and management of fever in the neonate and young infant (less than three months of age) [Electronic Version]. UpToDate,Teach, S.J., Kaplan, SL, Wiley, JF.
- ↑ Dagan, R. Sofer, S., Phillip, M., & Shachak, E. (1988). Ambulatory care of febrile infants younger than 2 months of age classified as being at low risk for having serous bacterial infections. Journal of Pediatrics, 112(3), 355-360.
- ↑ Evaluation and Management of Well-Appearing Febrile Infants 8 to 60 Days Old Robert H. Pantell, Kenneth B. Roberts, William G. Adams, Benard P. Dreyer, Nathan Kuppermann, Sean T. O'Leary, Kymika Okechukwu and Charles R. Woods; Subcommittee On Febrile Infants Pediatrics July 2021, e2021052228; DOI: https://doi.org/10.1542/peds.2021-052228