Diferencia entre revisiones de «Nontraumatic thoracic aortic dissection»
Sin resumen de edición |
|||
| (No se muestran 165 ediciones intermedias de 22 usuarios) | |||
| Línea 1: | Línea 1: | ||
''Not to be confused with [[traumatic aortic transection]]'' | |||
==Background== | ==Background== | ||
[[File:Aorta segments.jpg|thumb|Aortic segments]] | |||
[[File:Aorta branches.jpg|thumb|Branches of the aorta]] | |||
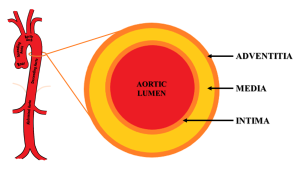
[[File:IJRRT-09-00343-g002.png|thumb|Aortic anatomy. The aorta is divided into 5 anatomical segments– aortic root, ascending aorta, aortic arch, descending thoracic aorta, and abdominal aorta. Its wall is composed of three layers – intima, media, and adventitia.]] | |||
*Most commonly seen in men 60-80 yrs old | |||
*Intimal tear with blood leaking into media | |||
*Mortality in first 48 hours of acute presentation is high | |||
**Commonly quoted as 1-2% per hour, but this is based on a series from the 1950s<ref>Hirst AE Jr, et al. Dissecting aneurysm of the aorta: a review of 505 cases. ''Medicine (Baltimore)''. 1958;37(3):217-279.</ref> | |||
**More recent data suggests mortality for type A dissection is 0.5% per hour when treated medically, and 0.1% per hour when managed surgically<ref>Harris, KM. et al. Early mortality in type A acute aortic dissection: Insights from the International Registry of Acute Aortic Dissection. ''JAMA Cardiol''. 2022;7(10):1009-1015.</ref> | |||
*Diagnosis delayed > 24hr in 50% of cases | |||
*Bimodal age distribution | |||
**Young with risk factors | |||
***[[Connective tissue disease]] (e.g. [[Marfan syndrome]], Ehlers-Danlos, collagen vascular disease) | |||
***[[Pregnancy]], especially 3rd trimester | |||
***Recent cardiac catheterization | |||
***Bicuspid aortic valve | |||
***[[coarctation of the Aorta|Aortic coarctation]] | |||
**Elderly males with chronic hypertension | |||
**Atherosclerotic risk factors (smoking, hypertension, HLD, DM) | |||
2- | ==Clinical Features== | ||
===General=== | |||
*Symptoms | |||
**Tearing/ripping [[chest pain|pain]] (10.8x increased disease probability) | |||
***64% described the pain as sharp vs 50.6% who described it as tearing or ripping<ref>Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903.</ref> | |||
**Migrating pain (7.6x) | |||
**Sudden chest pain (2.6x) | |||
**History of [[hypertension]] (1.5x) | |||
*Signs | |||
**[[Focal neuro deficit|Focal neurologic deficit]] (33x) | |||
**Diastolic heart [[murmur]] (acute aortic regurg) (4.9x) | |||
**Pulse deficit (2.7x) | |||
**[[Hypertension]] at time of presentation (49% of all cases<ref name="a">Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000; 283(7):897-903.</ref>) | |||
===Specific=== | |||
*Ascending Aorta | |||
**Acute [[aortic regurgitation]], leading to a diastolic decrescendo [[murmur]], [[hypotension]], or [[heart failure]], in 50%-66% | |||
**[[MI]]/Ischemia on ECG, usually inferior (dissection affects the right coronary artery more often than the left coronary artery<ref>Spittell PC, S et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990) Mayo Clin Proc. 1993;68:642–51.</ref>) | |||
**[[Cardiac Tamponade]] | |||
**[[Hemothorax]] - if adventitia disruption | |||
**[[Horner syndrome|Horners]], partial - sympathetic ganglion | |||
**Voice hoarseness - recurrent laryngeal nerve compression | |||
**[[CVA]]/[[Syncope]] - if carotid extension | |||
**[[Focal neuro deficit|Neurological deficits]] | |||
**SBP>20mmhg difference between arms | |||
**[[Hypertension]] at time of presentation (35.7% of all cases<ref name="a"/>) | |||
*Descending Aorta | |||
**[[Chest pain]], [[back pain]], [[abdominal pain]] | |||
***Pain abrupt, severe (90% of patients) radiating to back | |||
**[[Hypertension]] at time of presentation (70.1% of all cases<ref name="a" />) | |||
**[[Weakness|Hemiplegia]], neuropathy (15%) | |||
**[[Renal failure]] | |||
**Distal Pulse deficits/ [[limb ischemia]] | |||
**[[Mesenteric ischemia]] | |||
==Differential Diagnosis== | |||
{{Chest Pain DDX}} | |||
{{Hypertension DDX}} | |||
=== | ==Evaluation== | ||
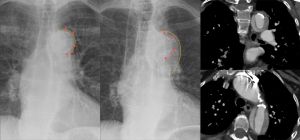
[[File:1920px-Dissektion im Aortenbogen im Roentgenbild 76W - CR und CT - 001 - Annotation.jpg|thumb|Dissection of the aortic arch in X-ray image 76W - CR and CT - 001 - Annotation.jpg|Dissection of the aortic arch: initial CXR normal visualization of the calcification shadow in the aortic arch (left); CXR 4 months later with calcification shifted centrally into the shadow of the aortic arch with a blurred external border (middle); CT scan coronal (top right) and axial (lower right).]] | |||
[[File:Dissection CXR.jpg|thumbnail|CXR showing widened mediastinum and porminent aortic knob]] | |||
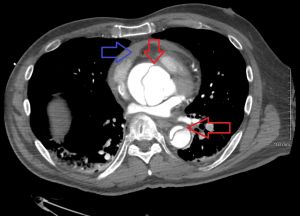
[[File:Dissection2018WithPericardial.jpg|thumb|Type A dissection with pericardial effusion as a result. Red arrows showing ascending and descending thoracic aorta. The blue arrows pericardial effusion.]] | |||
[[File:Dissection.png|thumbnail|CT chest with contrast of thoracic aortic dissection.]] | |||
===[https://www.mdcalc.com/aortic-dissection-detection-risk-score-add-rs Aortic Dissection Detection Risk Score (ADD-RS)]=== | |||
''A score 1 should be awarded for each of the 3 categories that contain at least one of the listed features'' | |||
{| class="wikitable" | |||
| align="center" style="background:#f0f0f0;"|'''Predisposing conditions''' | |||
| align="center" style="background:#f0f0f0;"|'''Pain features''' | |||
| align="center" style="background:#f0f0f0;"|'''Physical findings''' | |||
|- | |||
| | |||
*[[Marfan syndrome]] | |||
*[[Connective tissue disease]] | |||
*Family history of aortic disease | |||
*Recent aortic manipulation | |||
*Known thoracic aortic aneurysm | |||
|| | |||
Chest, back, or abdominal pain described as: | |||
*Abrupt in onset/severe in intensity | |||
AND | |||
*Ripping/tearing/sharp or stabbing quality | |||
|| | |||
*Evidence of perfusion deficit | |||
**Pulse deficit | |||
**Systolic BP differential | |||
**Focal neurological deficit (in conjunction with pain) | |||
*Murmur of aortic insufficiency (new or not known to be old and in conjunction with pain) | |||
*[[Hypotension]] of shock state | |||
|} | |||
{| class="wikitable" | |||
| align="center" style="background:#f0f0f0;"|'''Score''' | |||
| align="center" style="background:#f0f0f0;"|'''Category''' | |||
| align="center" style="background:#f0f0f0;"|'''Prevalence''' | |||
|- | |||
| 0||Low||6% | |||
|- | |||
| 1||Intermediate||27% | |||
|- | |||
| >1||High||39% | |||
|} | |||
===No Risk Factor Screening=== | |||
*[[CXR]] | |||
**Abnormal in 90% (3.4x) | |||
**Mediastinal widening (seen in 56-63%) | |||
**Left sided pleural effusion (seen in 19%) | |||
**Widening of aortic contour (seen in 48%), displaced calcification (6mm), Calcium sign (look for white line of calcium within aortic knob and measure to outer edge of the aortic knob - distance greater than 0.5 cm is positive and > 1 cm is highly suspicious for dissection), aortic kinking, double density sign | |||
===Low-Intermediate=== | |||
''(Based on ADD-RS)''<ref>Circulation. 2018 Jan 16;137(3):250-258. doi: 10.1161/CIRCULATIONAHA.117.029457. Epub 2017 Oct 13. Nazerian, et al. Diagnostic Accuracy of the Aortic Dissection Detection Risk Score Plus D-Dimer for Acute Aortic Syndromes: The ADvISED Prospective Multicenter Study.</ref><ref>Asha SE et al. "A systematic review and meta-analysis of D-dimer as a rule out test for suspected acute aortic dissection." Annals of EM. 66;4;368-377Ocotber 2015.</ref><ref>Shimony A, et al. Meta-analysis of usefulness of d-dimer to diagnose acute aortic dissection. Am J Cardiol. 2011; 107(8):1227-1234.</ref> | |||
*[[D-dimer]] for ADD-RS ≤ 1 (low or intermediate risk) | |||
===High Risk/Definitive=== | |||
*CT aortogram chest | |||
**Study of choice | |||
**Similar sensitivity/specificity to TEE and MRA | |||
*TEE | |||
**If CT delayed due to contrast allergy or availability, or patient instability. | |||
**TEE has a sensitivity of 98% and 95% specific<ref>Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y. Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection: systematic review and meta-analysis. Arch Intern Med. 2006 Jul 10;166(13):1350-6.</ref> | |||
Type | ===Other Findings=== | ||
[[File:aorticdissection.gif|thumbnail|Type A Aortic Dissection<ref>http://www.thepocusatlas.com/echocardiography-1</ref>]] | |||
[[File:USDissection.png|thumbnail|Abdominal Aortic Dissection on Ultrasound]] | |||
*[[ECG]] | |||
**[[LVH]] on admission ECG (3.2x) | |||
**Ischemia (esp inferior) - 15% | |||
**Nonspec ST-T changes - 40% | |||
*[[echocardiography|Bedside US]] | |||
**Can help in ruling in patients when AOFT is >4cm | |||
**Rule out pericardial effusion and tamponade, especially in hypotension, syncope, dyspnea | |||
{{Aortic dissection classification}} | |||
==Management== | |||
===General Principles=== | |||
*Control pain to reduce sympathetic stimulation. | |||
**[[Fentanyl]] is easily titratable with minimal cardiovascular effects | |||
*Right radial arterial line or right arm blood pressure will generally be the most accurate | |||
*Reducing heart rate while maintaining low-normal blood pressure reduces aortic flow acceleration, thereby reducing shear force on the intimal wall | |||
**'''Goal: HR < 60 bpm, SBP 100-120 mmHg''' | |||
**Control heart rate before blood pressure<ref>[https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.105.534198 Tsai TT, Nienaber CA, and Eagle KA. Acute Aortic Syndromes. Circulation. 2005;112:3802–3813]</ref> | |||
**[[Beta blockers]] are good first-line option, since they reduce heart rate and aortic wall tension | |||
***Use β-blockers with caution in severe, acute [[aortic regurgitation]] - may worsen shock if dependent on compensatory tachycardia | |||
===Heart Rate control=== | |||
#[[Esmolol]] | |||
#*Advantage of short half life, easily titratable | |||
#*Bolus 0.5mg/kg over 1min; infuse 0.05mg/kg/min (titrate upward in 0.05mg/kg/min increments to a maximum of 0.3 mg/kg/min) | |||
#*[http://emcrit.org/wp-content/uploads/2013/01/esmolol-drip-sheet.pdf Esmolol Drip Sheet] | |||
#[[Labetalol]] - has both α and beta effects | |||
#*Push dose - 10-20mg with repeat doses of 20-40mg q10min up to 300mg | |||
#*Drip - Load 15-20mg IV, followed by 5mg/hr | |||
#[[Metoprolol]] | |||
#*5mg IV x 3; infuse at 2-5mg/hr | |||
#[[Diltiazem]] - Use if contraindications to beta-blockers | |||
#*Loading 0.25mg/kg over 2–5 min, followed by a drip of 5mg/h | |||
== | ===Blood pressure control (vasodilators)=== | ||
Use if needed after beta-blockade. | |||
#[[Nicardipine]]: | |||
#*5mg/hr start, then titrate up by 2.5mg/hr every 10 min until goal | |||
#*Once at goal, drop to 3mg/hr and re-titrate from there | |||
#*May initially bolus 2mg IV<ref>Curran MP et al. Intravenous Nicardipine. Drugs 2006; 66(13): 1755-1782. http://emcrit.org/wp-content/uploads/2014/07/bolus-dose-nicardipine.pdf</ref> | |||
#[[Clevidipine]] | |||
#*1-2 mg/hr | |||
#*Double dose every 90 seconds until approaching goal BP, then increase in smaller amounts every 5-10 minutes until goal achieved.<ref>UpToDate Inc. Clevidipine [Drug information]. In:UpToDate Lexidrug. Wolters Kluwer; 2025. Accessed August 1, 2025.</ref> | |||
#[[Nitroprusside]] 0.3-0.5mcg/kg/min - Risk of cerebral blood vessel vasodilation and CN/Thiocynate toxicity | |||
#[[Fenoldopam]] | |||
#[[Enalapril]] | |||
===Surgery=== | |||
*Type A (any portion of ascending aorta) | |||
**Requires surgery | |||
*Type B (isolated to descending aorta) | |||
**Primarily medical management with surgery consultation | |||
=== | ==Disposition== | ||
*Admission to OR or ICU | |||
* | |||
==Complications== | ==Complications== | ||
*AV Regurgitation/Insufficiency | |||
**[[CHF]] with diastolic murmur | |||
*Rupture | |||
**Pericardium: [[cardiac tamponade]] | |||
**Mediastinum: [[hemothorax]] | |||
*Vascular obstruction | |||
**Coronary: [[ACS]] | |||
**Carotid: [[CVA]] | |||
**Lumbar: Paraplegia | |||
==See Also== | |||
*[[Hypertensive emergency]] | |||
*[[Traumatic aortic transection]] | |||
*[[Abdominal aortic aneurysm]] | |||
*[[IRAD]] | |||
== | |||
== | ==External Links== | ||
*[http://www.thennt.com/lr/aortic-dissection/ NNT Aortic Dissection LRs] | |||
*[http://circ.ahajournals.org/content/121/13/e266.full AHA Full Guidelines] | |||
*[http://emupdates.com/2010/06/23/accaha-aortic-dissection-guideline/ AHA Quick Summary] | |||
*[http://academiclifeinem.com/paucis-verbis-international-registry-on-aortic-dissection-irad/ ALiEM Paucis Verbis: International Registry on Aortic Dissection (IRAD)] | |||
*[https://www.mdcalc.com/aortic-dissection-detection-risk-score-add-rs#evidence MDcalc ADD Score] | |||
==References== | |||
<references/> | |||
[[Category: | [[Category:Cardiology]] | ||
[[Category:Vascular]] | |||
Revisión actual - 19:44 17 sep 2025
Not to be confused with traumatic aortic transection
Background
- Most commonly seen in men 60-80 yrs old
- Intimal tear with blood leaking into media
- Mortality in first 48 hours of acute presentation is high
- Diagnosis delayed > 24hr in 50% of cases
- Bimodal age distribution
- Young with risk factors
- Connective tissue disease (e.g. Marfan syndrome, Ehlers-Danlos, collagen vascular disease)
- Pregnancy, especially 3rd trimester
- Recent cardiac catheterization
- Bicuspid aortic valve
- Aortic coarctation
- Elderly males with chronic hypertension
- Atherosclerotic risk factors (smoking, hypertension, HLD, DM)
- Young with risk factors
Clinical Features
General
- Symptoms
- Tearing/ripping pain (10.8x increased disease probability)
- 64% described the pain as sharp vs 50.6% who described it as tearing or ripping[3]
- Migrating pain (7.6x)
- Sudden chest pain (2.6x)
- History of hypertension (1.5x)
- Tearing/ripping pain (10.8x increased disease probability)
- Signs
- Focal neurologic deficit (33x)
- Diastolic heart murmur (acute aortic regurg) (4.9x)
- Pulse deficit (2.7x)
- Hypertension at time of presentation (49% of all cases[4])
Specific
- Ascending Aorta
- Acute aortic regurgitation, leading to a diastolic decrescendo murmur, hypotension, or heart failure, in 50%-66%
- MI/Ischemia on ECG, usually inferior (dissection affects the right coronary artery more often than the left coronary artery[5])
- Cardiac Tamponade
- Hemothorax - if adventitia disruption
- Horners, partial - sympathetic ganglion
- Voice hoarseness - recurrent laryngeal nerve compression
- CVA/Syncope - if carotid extension
- Neurological deficits
- SBP>20mmhg difference between arms
- Hypertension at time of presentation (35.7% of all cases[4])
- Descending Aorta
- Chest pain, back pain, abdominal pain
- Pain abrupt, severe (90% of patients) radiating to back
- Hypertension at time of presentation (70.1% of all cases[4])
- Hemiplegia, neuropathy (15%)
- Renal failure
- Distal Pulse deficits/ limb ischemia
- Mesenteric ischemia
- Chest pain, back pain, abdominal pain
Differential Diagnosis
Chest pain
Critical
- Acute coronary syndromes (ACS)
- Aortic dissection
- Cardiac tamponade
- Coronary artery dissection
- Esophageal perforation (Boerhhaave's syndrome)
- Pulmonary embolism
- Tension pneumothorax
Emergent
- Cholecystitis
- Cocaine-associated chest pain
- Mediastinitis
- Myocardial rupture
- Myocarditis
- Pancreatitis
- Pericarditis
- Pneumothorax
Nonemergent
- Aortic stenosis
- Arthritis
- Asthma exacerbation
- Biliary colic
- Costochondritis
- Esophageal spasm
- Gastroesophageal reflux disease
- Herpes zoster / Postherpetic Neuralgia
- Hypertrophic cardiomyopathy
- Hyperventilation
- Mitral valve prolapse
- Panic attack
- Peptic ulcer disease
- Pleuritis
- Pneumomediastinum
- Pneumonia
- Rib fracture
- Stable angina
- Thoracic outlet syndrome
- Valvular heart disease
- Muscle sprain
- Psychologic / Somatic Chest Pain
- Spinal Root Compression
- Tumor
Hypertension
- Hypertensive emergency
- Stroke
- Sympathetic crashing acute pulmonary edema
- Ischemic stroke
- Intracranial hemorrhage
- Preeclampsia/Eclampsia
- Autonomic dysreflexia
- Scleroderma renal crisis
- Acute glomerulonephritis
- Type- I myocardial infarction
- Volume overload
- Urinary obstruction
- Drug use or overdose (e.g stimulants, especially alcohol, cocaine, or Synthroid)
- Renal Artery Stenosis
- Nephritic and nephrotic syndrome
- Polycystic kidney disease
- Tyramine reaction
- Cushing's syndrome
- Obstructive sleep apnea
- Pheochromocytoma
- Hyperaldosteronism
- Hyperthyroidism
- Anxiety
- Pain
- Oral contraceptive use
Evaluation
Dissection of the aortic arch: initial CXR normal visualization of the calcification shadow in the aortic arch (left); CXR 4 months later with calcification shifted centrally into the shadow of the aortic arch with a blurred external border (middle); CT scan coronal (top right) and axial (lower right).
Aortic Dissection Detection Risk Score (ADD-RS)
A score 1 should be awarded for each of the 3 categories that contain at least one of the listed features
| Predisposing conditions | Pain features | Physical findings |
|
Chest, back, or abdominal pain described as:
AND
|
|
| Score | Category | Prevalence |
| 0 | Low | 6% |
| 1 | Intermediate | 27% |
| >1 | High | 39% |
No Risk Factor Screening
- CXR
- Abnormal in 90% (3.4x)
- Mediastinal widening (seen in 56-63%)
- Left sided pleural effusion (seen in 19%)
- Widening of aortic contour (seen in 48%), displaced calcification (6mm), Calcium sign (look for white line of calcium within aortic knob and measure to outer edge of the aortic knob - distance greater than 0.5 cm is positive and > 1 cm is highly suspicious for dissection), aortic kinking, double density sign
Low-Intermediate
- D-dimer for ADD-RS ≤ 1 (low or intermediate risk)
High Risk/Definitive
- CT aortogram chest
- Study of choice
- Similar sensitivity/specificity to TEE and MRA
- TEE
- If CT delayed due to contrast allergy or availability, or patient instability.
- TEE has a sensitivity of 98% and 95% specific[9]
Other Findings

Type A Aortic Dissection[10]
- ECG
- LVH on admission ECG (3.2x)
- Ischemia (esp inferior) - 15%
- Nonspec ST-T changes - 40%
- Bedside US
- Can help in ruling in patients when AOFT is >4cm
- Rule out pericardial effusion and tamponade, especially in hypotension, syncope, dyspnea
Aortic Dissection Classification
- Stanford
- Type A: Involves any portion of ascending aorta
- Type B: Isolated to descending aorta
- De Bakey
- Type I: Involves the ascending and descending aorta
- Type II: Involves only the ascending aorta
- Type III: Involves only the descending aorta
| Image | 
|

|

|
| Percentage | 60% | 10–15% | 25–30% |
| Type | DeBakey I | DeBakey II | DeBakey III |
| Classification | Stanford A (Proximal) | Stanford B (Distal) | |
Management
General Principles
- Control pain to reduce sympathetic stimulation.
- Fentanyl is easily titratable with minimal cardiovascular effects
- Right radial arterial line or right arm blood pressure will generally be the most accurate
- Reducing heart rate while maintaining low-normal blood pressure reduces aortic flow acceleration, thereby reducing shear force on the intimal wall
- Goal: HR < 60 bpm, SBP 100-120 mmHg
- Control heart rate before blood pressure[11]
- Beta blockers are good first-line option, since they reduce heart rate and aortic wall tension
- Use β-blockers with caution in severe, acute aortic regurgitation - may worsen shock if dependent on compensatory tachycardia
Heart Rate control
- Esmolol
- Advantage of short half life, easily titratable
- Bolus 0.5mg/kg over 1min; infuse 0.05mg/kg/min (titrate upward in 0.05mg/kg/min increments to a maximum of 0.3 mg/kg/min)
- Esmolol Drip Sheet
- Labetalol - has both α and beta effects
- Push dose - 10-20mg with repeat doses of 20-40mg q10min up to 300mg
- Drip - Load 15-20mg IV, followed by 5mg/hr
- Metoprolol
- 5mg IV x 3; infuse at 2-5mg/hr
- Diltiazem - Use if contraindications to beta-blockers
- Loading 0.25mg/kg over 2–5 min, followed by a drip of 5mg/h
Blood pressure control (vasodilators)
Use if needed after beta-blockade.
- Nicardipine:
- 5mg/hr start, then titrate up by 2.5mg/hr every 10 min until goal
- Once at goal, drop to 3mg/hr and re-titrate from there
- May initially bolus 2mg IV[12]
- Clevidipine
- 1-2 mg/hr
- Double dose every 90 seconds until approaching goal BP, then increase in smaller amounts every 5-10 minutes until goal achieved.[13]
- Nitroprusside 0.3-0.5mcg/kg/min - Risk of cerebral blood vessel vasodilation and CN/Thiocynate toxicity
- Fenoldopam
- Enalapril
Surgery
- Type A (any portion of ascending aorta)
- Requires surgery
- Type B (isolated to descending aorta)
- Primarily medical management with surgery consultation
Disposition
- Admission to OR or ICU
Complications
- AV Regurgitation/Insufficiency
- CHF with diastolic murmur
- Rupture
- Pericardium: cardiac tamponade
- Mediastinum: hemothorax
- Vascular obstruction
See Also
External Links
- NNT Aortic Dissection LRs
- AHA Full Guidelines
- AHA Quick Summary
- ALiEM Paucis Verbis: International Registry on Aortic Dissection (IRAD)
- MDcalc ADD Score
References
- ↑ Hirst AE Jr, et al. Dissecting aneurysm of the aorta: a review of 505 cases. Medicine (Baltimore). 1958;37(3):217-279.
- ↑ Harris, KM. et al. Early mortality in type A acute aortic dissection: Insights from the International Registry of Acute Aortic Dissection. JAMA Cardiol. 2022;7(10):1009-1015.
- ↑ Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000;283(7):897–903.
- ↑ 4.0 4.1 4.2 Hagan PG, Nienaber CA, Isselbacher EM, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000; 283(7):897-903.
- ↑ Spittell PC, S et al. Clinical features and differential diagnosis of aortic dissection: experience with 236 cases (1980 through 1990) Mayo Clin Proc. 1993;68:642–51.
- ↑ Circulation. 2018 Jan 16;137(3):250-258. doi: 10.1161/CIRCULATIONAHA.117.029457. Epub 2017 Oct 13. Nazerian, et al. Diagnostic Accuracy of the Aortic Dissection Detection Risk Score Plus D-Dimer for Acute Aortic Syndromes: The ADvISED Prospective Multicenter Study.
- ↑ Asha SE et al. "A systematic review and meta-analysis of D-dimer as a rule out test for suspected acute aortic dissection." Annals of EM. 66;4;368-377Ocotber 2015.
- ↑ Shimony A, et al. Meta-analysis of usefulness of d-dimer to diagnose acute aortic dissection. Am J Cardiol. 2011; 107(8):1227-1234.
- ↑ Shiga T, Wajima Z, Apfel CC, Inoue T, Ohe Y. Diagnostic accuracy of transesophageal echocardiography, helical computed tomography, and magnetic resonance imaging for suspected thoracic aortic dissection: systematic review and meta-analysis. Arch Intern Med. 2006 Jul 10;166(13):1350-6.
- ↑ http://www.thepocusatlas.com/echocardiography-1
- ↑ Tsai TT, Nienaber CA, and Eagle KA. Acute Aortic Syndromes. Circulation. 2005;112:3802–3813
- ↑ Curran MP et al. Intravenous Nicardipine. Drugs 2006; 66(13): 1755-1782. http://emcrit.org/wp-content/uploads/2014/07/bolus-dose-nicardipine.pdf
- ↑ UpToDate Inc. Clevidipine [Drug information]. In:UpToDate Lexidrug. Wolters Kluwer; 2025. Accessed August 1, 2025.