Diferencia entre revisiones de «Hip dislocation»
(Text replacement - "Category:Ortho" to "Category:Orthopedics") |
(Post Hip reduction care) |
||
| Línea 40: | Línea 40: | ||
===Anterior=== | ===Anterior=== | ||
*Reduction: traction, internal rotation, and then external rotation once the femoral hip clears the acetabular rim | *Reduction: traction, internal rotation, and then external rotation once the femoral hip clears the acetabular rim | ||
==Post Reduction Care== | |||
*Maintain dislocation precautions: | |||
**Do not bend the operated hip past 90 degrees. | |||
**Do not cross the midline of the body with operated leg. | |||
**Do not rotate the operated leg inward. | |||
**In bed, toes and knee cap should point toward ceiling. | |||
*For unstable hips, consider bracing and hip abduction pillow | |||
*Toe touch weight bearing | |||
==Complications== | ==Complications== | ||
Revisión del 23:31 4 may 2016
Background
- Orthopedic emergency; reduction should occur w/in 6hr due to high risk of AVN
- High-energy trauma is primary mechanism
Types
- Posterior
- 90% of hip dislocations
- Acetabular fractures may result as well
- Anterior
- 10% of hip dislocations[1]
- Can be superior (pelvic) or inferior (obturator)
- Neurovascular compromise is unusual
Clinical Features
- Posterior Dislocation
- Extremity is shortened, internally rotated, adducted
- Often Knee-to-Dashboard
- Assess neurovascular exam
- Sciatic nerve is most common compromised
- Anterior Dislocation
- Extremity is extended (superior) or flexed (inferior), externally rotated, abducted[2]
- Similar to hip fracture
Differential Diagnosis
Hip pain
Acute Trauma
- Femur fracture
- Proximal
- Intracapsular
- Extracapsular
- Shaft
- Mid-shaft femur fracture (all subtrochanteric)
- Proximal
- Hip dislocation
- Pelvic fractures
Chronic/Atraumatic
- Hip bursitis
- Psoas abscess
- Piriformis syndrome
- Meralgia paresthetica
- Septic arthritis
- Obturator nerve entrapment
- Avascular necrosis of hip
Diagnosis
- Hip AP and lateral views
- Posterior Dislocation: AP view femoral head posterior and superior to acetabulum
- Anterior Dislocation: AP view shows femoral head in obturator foramen (inferior to acetabulum)
- Consider Judet views
- Consider knee xray
- Consider CT to evaluate acetabulum for subtle fractures (esp for posterior dislocation)
Management
Reduction recommended within 6 hours to prevent avascular necrosis of the femoral head[3]
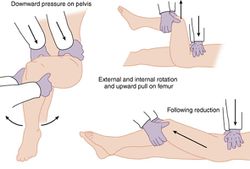
Posterior
- Allis Maneuver: supine patient on table: deeper sedation (propofol helps with tissue relaxation); firm distal traction at flexed knee to pull head back into acetabulum; assistant stabilizes pelvis by pushing on ASISs
Anterior
- Reduction: traction, internal rotation, and then external rotation once the femoral hip clears the acetabular rim
Post Reduction Care
- Maintain dislocation precautions:
- Do not bend the operated hip past 90 degrees.
- Do not cross the midline of the body with operated leg.
- Do not rotate the operated leg inward.
- In bed, toes and knee cap should point toward ceiling.
- For unstable hips, consider bracing and hip abduction pillow
- Toe touch weight bearing
Complications
- Post-traumatic arthritis
- 20% in simple dislocations
- high in complex dislocations
- Femoral head osteonecrosis
- 5-40% incidence
- Delay in treatment >6 hours can lead to avascular necrosis of the femoral head => osteonecrosis
- Sciatic nerve injury
- 8-20% incidence
- associated with longer time to reduction
- Recurrent dislocations: <2%
References
- ↑ Holt GE and McCarty EC. Anterior hip dislocation with an associated vascular injury requiring amputation. J Trauma. 2003; 55(1):135-138.
- ↑ Alonso JE, et al. A review of the treatment of hip dislocations associated with acetabular fractures. Clin Orthop Relat Res. 2000; 377(8):32-43.
- ↑ Jaskulka RA, et al. Dislocation and fracture-dislocation of the hip. J Bone Joint Surg Br. 1991; 73(3):465-469.