Diferencia entre revisiones de «Hip dislocation»
(additional citations/evidence) |
(added complications section) |
||
| Línea 34: | Línea 34: | ||
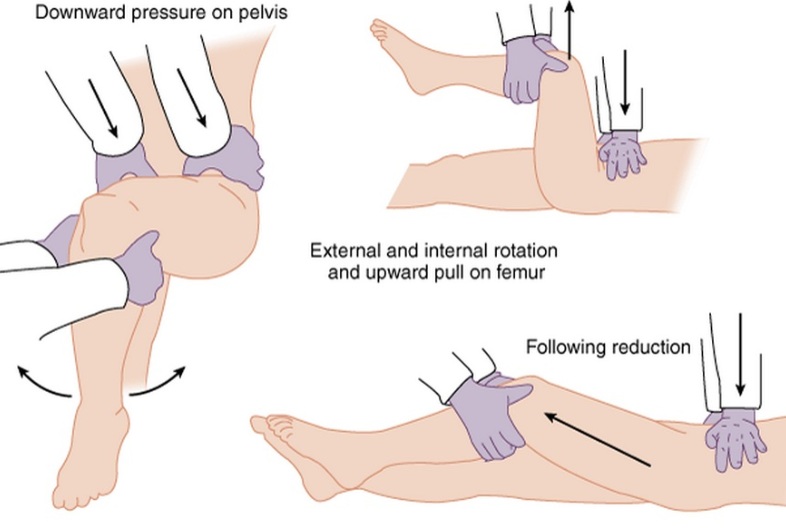
[[File:Hip_Reduction.jpg]] | [[File:Hip_Reduction.jpg]] | ||
==Complications== | |||
*Post-traumatic arthritis | |||
**20% in simple dislocations | |||
**high in complex dislocations | |||
*Femoral head osteonecrosis | |||
**5-40% incidence | |||
**Increased risk with increased time to reduction | |||
*Sciatic nerve injury | |||
**8-20% incidence | |||
**associated with longer time to reduction | |||
*Recurrent dislocations: <2% | |||
==Source== | ==Source== | ||
Revisión del 15:12 29 dic 2014
Background
- Orthopedic emergency; reduction should occur w/in 6hr
- High risk of AVN
- High-energy trauma is primary mechanism
- Types:
- Posterior
- 90% of hip dislocations
- Acetabular fractures may result as well
- Anterior
- 10% of hip dislocations
- Can be superior (pelvic) or inferior (obturator)
- Neurovascular compromise is unusual
- Posterior
Clinical Features
- Posterior Dislocation
- Extremity is shortened, internally rotated, adducted
- Often Knee-to-Dashboard
- Anterior Dislocation
- Extremity is flexed, externally rotated, abducted
- Similar to hip fracture
Imaging
- Hip AP and lateral views
- Posterior Dislocation: AP view femoral head posterior and superior to acetabulum
- Anterior Dislocation: AP view shows femoral head in obturator foramen (inferior to acetabulum)
- Also consider Judet views or CT to evaluate acetabulum (esp for posterior dislocation)
Management
- Reduce
- Posterior
- Allis Maneuver: supine patient on table: deeper sedation (propofol helps with tissue relaxation); firm distal traction at flexed knee to pull head back into acetabulum; assistant stabilizes pelvis by pushing on ASISs
- Anterior
- Reduction: traction, internal rotation, and then external rotation once the femoral hip clears the acetabular rim
- Posterior
Complications
- Post-traumatic arthritis
- 20% in simple dislocations
- high in complex dislocations
- Femoral head osteonecrosis
- 5-40% incidence
- Increased risk with increased time to reduction
- Sciatic nerve injury
- 8-20% incidence
- associated with longer time to reduction
- Recurrent dislocations: <2%
Source
- Tintinalli
- Review of Orthopaedics, 6th Edition, Mark D. Miller MD, Stephen R. Thompson MBBS MEd FRCSC, Jennifer Hart MPAS PA-C ATC, an imprint of Elsevier, Philadelphia, Copyright 2012
- AAOS Comprehensive Orthopaedic Review, Jay R. Leiberman. Published by American Academy of Orthopaedic Surgeons, Rosemont IL. Copyright 2009